
Inside the
ADHD brain
Explore the latest science on how 3 neurotransmitters may serve an important role in the symptoms of ADHD1,2
Explore the latest science on how 3 neurotransmitters may play a role in ADHD1,2
While the roles of dopamine (DA) and norepinephrine (NE) in ADHD are well studied, recent evidence suggests that serotonin (5-HT) may be pivotal in both the diagnostic symptoms and associated symptoms of ADHD—such as emotional dysregulation and executive dysfunction—in addition to frequently co-occurring conditions like depression and anxiety.1-3 The interplay between these neurotransmitters may be responsible for the heterogeneity of ADHD symptoms within patients.4,5
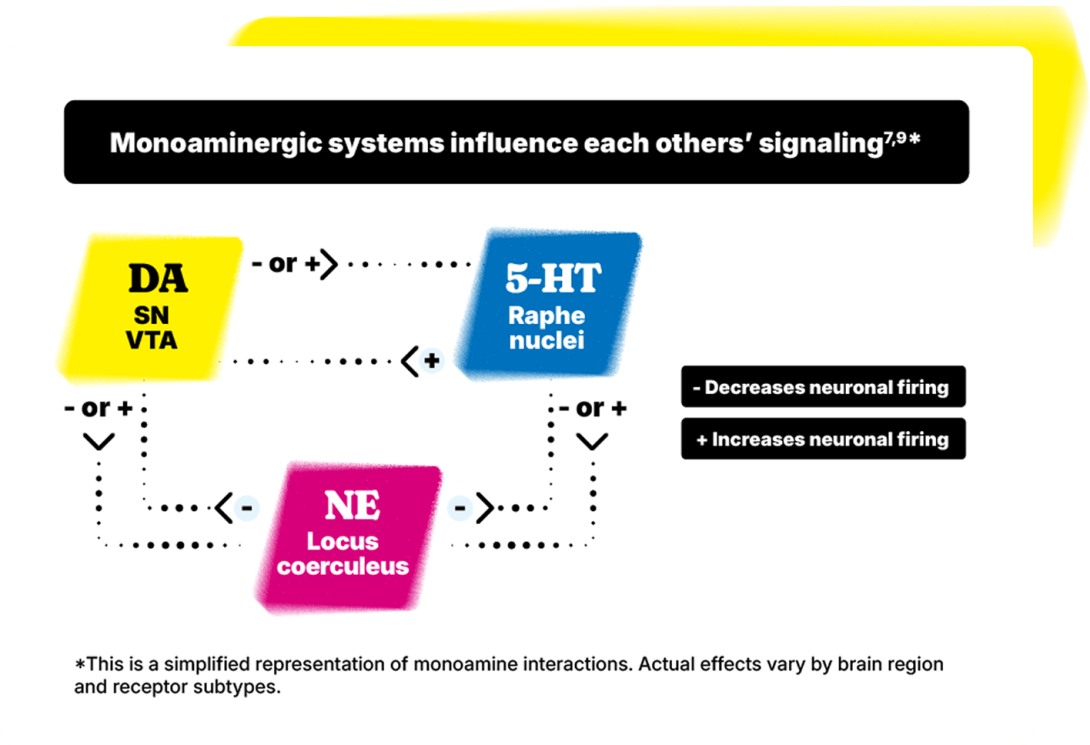
Interactions among the 3 neurotransmitters are complex1,6,7
Reciprocal projections among NE, DA, and 5-HT neurons exist throughout the brain. Attempts to enhance transmission of 1 monoamine system can lead to a decrease in function of others.8
The roles of NE, DA, and 5-HT in the symptoms of ADHD often overlap1,6,7
The overlapping symptoms in bold below illustrate the complex neurobiology of ADHD, involving multiple pathophysiological pathways in the brain.1,6,7
The noradrenergic system is thought to play a role in:1,2,7
- Attention
- Mood
- Regulation in cognitive functions
- Arousal
- Signal-to-noise processing
- Stress response
The dopaminergic system is thought to play a role in:1
- Attention
- Mood
- Reward processing
- Cognitive processes
- Regulation of movement
- Learning and memory
The serotoninergic system is thought to play a role in:1–3
- Mood
- Reward processing
- Emotional regulation
- Executive control
- Impulse control
Associated symptoms and comorbidities
NE, DA, and 5-HT are likely to contribute to emotional dysregulation and executive dysfunction.1-3The dysregulation of these neurotransmitters has been linked to depression and anxiety.1
Dive deeper into how neurotransmitters may play a role in the symptoms of ADHD
The interplay of NE, DA, and 5-HT is present across multiple brain regions implicated in ADHD
- Connections within and between key brain networks thought to be involved in ADHD are modulated by monoaminergic inputs7
- 5-HT modulates DA activity in the prefrontal cortex and nucleus accumbens/striatum, impacting key regions involved in both diagnostic (impulsivity and inattention) and associated symptoms (mood, cognition, sleep) of ADHD7,10-12
- NE/DA play a complementary and critical role in prefrontal cortex function7,10-12
These brain regions play many roles, including some that are thought to be related to ADHD7
Prefrontal cortex
- Working memory
- Planning
- Selective attention
Parietal cortex
- Attention
- Cognitive flexibility
Anterior cingulate cortex
- Mood
- Cognitive aspects of executive control, attention, cognition
Amygdala
- Emotion
- Reward processing
Ventral striatum/basal ganglia
- Reward processing
- Motivation

Request a medical science liaison
Connect with an Otsuka Medical Science Liaison for access to clinical research and disease area education.

get curious about ASSOCIATED SYMPTOMS
Explore resources to help better understand the impact of associated symptoms

Our understanding of ADHD is always evolving
Get the latest insights and resources delivered right to your inbox
-
1.
Faraone SV, et al. Larsson H. Genetics of attention deficit hyperactivity disorder. Mol Psychiatry. 2019;24:562-575.
-
2.
da Silva BS, et al. An overview on neurobiology and therapeutics of attention‑deficit/
hyperactivity disorder. Disc Mental Health. 2023;3(1):1-21. -
3.
Shaw P, et al. Emotional dysregulation in attention-deficit/hyperactivity disorder. Am J Psychiatry. 2014;171(3):276-293.
-
4.
Sonuga-Barke EJS, et al. Annual research review: perspectives on progress in ADHD science—from characterisation to cause. J Child Psychol Psychiatry. 2023;64(4):506-532.
-
5.
Banerjee E, Nandagopal K. Does serotonin deficit mediate susceptibility to ADHD? Neurochem Int. 2015;82:52-68.
-
6.
Hilger K, Fiebach CJ. ADHD symptoms are associated with the modular structure of intrinsic brain networks in a representative sample of healthy adults. Netw Neurosci. 2019;3(2):567-88.
-
7.
Faraone SV, et al. Attention-deficit/hyperactivity disorder. Nat Rev Dis Primers. 2024;10(11):1-21.
-
8.
Blier P. Rational site-directed pharmacotherapy for major depressive disorder. Int J Neuropsychopharmacol. 2014;17(7):997-1008.
-
9.
Guiard BP, et al. Functional interactions between dopamine, serotonin and norepinephrine neurons: an in-vivo electrophysiological study in rats with monoaminergic lesions. Int J Neuropsychopharmacol. 2008;11(5):625-639.
-
10.
Pourhamzeh M, et al. The roles of serotonin in neuropsychiatric disorders. Cell Mol Neurobiol. 2022;42(6):1671-92
-
11.
Madhyastha A, et al. Serotonergic and adrenergic neuroreceptor manipulation ameliorates core symptoms of ADHD through modulating dopaminergic receptors in spontaneously hypertensive rats. Int J Mol Sci. 2024;25(4):2300.
-
12.
Conio B, et al. Opposite effects of dopamine and serotonin on resting-state networks: review and implications for psychiatric disorder. Mol Psychiatry. 2020;25(1):82-93.
