
The full toll
of living with
ADHD
See how diagnostic symptoms, associated symptoms, and comorbidities may impact patients.
Symptoms in check. Sort of.
Even when the diagnostic symptoms of ADHD are managed, associated symptoms and comorbidities may leave patients with unmet needs.1
The full clinical presentation of ADHD may include not only diagnostic symptoms, but ADHD-associated symptoms as well, which can be a continuing source of struggle for patients.1-3
In addition, comorbidities such as anxiety and depression can further add to the full burden of ADHD.4,5 Patients may be left wondering: Is it me or my ADHD?
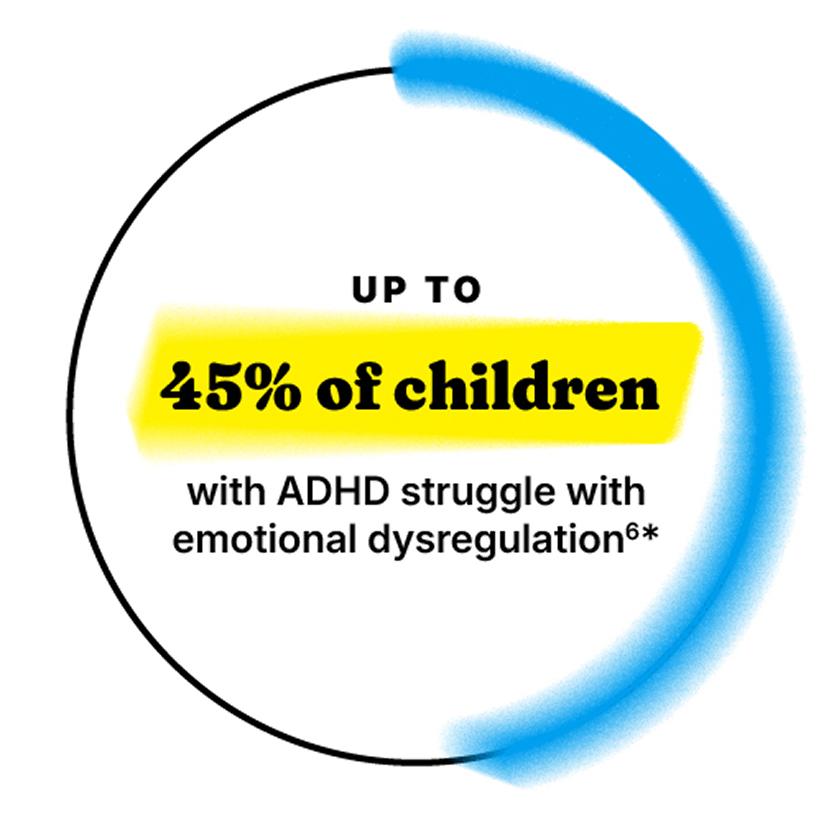
*Clinic-based studies in children ages 4–18 with ADHD have reported emotional dysregulation prevalence estimates of 24%–45%.
Difficulties with associated symptoms of ADHD can show up in many ways, including:
Low self-esteem7
Educational difficulties8,9
Social problems10
Employment problems11-13
Financial problems8,14,15
In addition, comorbidities, such as anxiety and depression, have overlapping symptoms that can blur the line between ADHD and other mental health disorders, complicating the lives of patients and the ability of providers to fully treat ADHD.4,5
Get the whole picture
Even when treated, ADHD leads to chronic social, occupational, interpersonal, and health challenges that cause a ripple effect within families and communities.1
A patient’s diagnostic symptoms may seem under control, but it’s important to ask patients if they’re struggling with associated symptoms as well.
The diagnostic criteria for ADHD16
Healthcare providers use the guidelines in the American Psychiatric Association’s Diagnostic and Statistical Manual, 5th edition, text revision
A minimum number of diagnostic
symptoms must be met
6 or more symptoms of inattention and/or hyperactivity/impulsivity for children up to age 16 years
5 or more symptoms of inattention and/or hyperactivity/impulsivity for adolescents aged 17 years and older and adults
Diagnostic symptoms are categorized into 2 buckets
Inattention
- Difficulty sustaining attention on tasks or activities
- Frequent careless mistakes due to inattention
- Seeming not to listen when spoken to directly
- Failure to follow through on instructions and tasks
- Trouble organizing tasks and activities
- Avoidance or dislike of sustained mental effort tasks
- Losing items necessary for tasks or activities
- Easily distracted by external stimuli
- Forgetfulness in daily activities
Hyperactivity/impulsivity
- Fidgeting or tapping hands/feet
- Inability to stay seated
- Running or climbing inappropriately (or restlessness in adults)
- Inability to play or engage in activities quietly
- Acting as if “driven by a motor”; difficulty remaining still
- Excessive talking
- Blurting out answers or interrupting conversations
- Difficulty waiting their turn
- Interrupting or intruding on others’ activities or conversations
Additional conditions must be met
- Several inattentive or hyperactive-impulsive symptoms were present before age 12 years
- Several symptoms are present in 2 or more settings (such as at home, school or work; with friends or relatives; in other activities)
- There is clear evidence that the symptoms interfere with, or reduce the quality of, social, school, or work functioning
- The symptoms are not better explained by another mental disorder (such as a mood disorder, anxiety disorder, dissociative disorder, or a personality disorder). The symptoms do not happen only during the course of schizophrenia or another psychotic disorder
An ADHD diagnosis could fall into 1 of these 3 presentations
Predominantly inattentive presentation (e.g., challenges with staying on task, focusing, and organization)
Predominantly hyperactive-impulsive presentation (e.g. excessive movement and energy, being talkative, decisions or actions taken without thinking through the consequences)
Combined presentation (ADHD with symptoms that fall into both categories)
Associated symptoms can also disrupt patients’ lives16
While diagnostic symptoms may be the most discernable symptoms of ADHD, associated symptoms are common and are listed in the DSM-5-TR to provide context and to support a clinical classification of ADHD. They may come up when a patient describes their experience. While they are separate from the diagnostic symptoms, they can exacerbate the impairment patients with ADHD already face.10,16
Emotional dysregulation
- Mood swings
- Irritability or frustration intolerance
- Difficulty managing stress
Executive dysfunction
- Problems with planning, prioritizing, and time management
- Poor working memory
Social challenges
- Difficulty maintaining relationships
- Misinterpreting social cues
- Low self-esteem due to repeated academic, social, or occupational struggles
Patients may struggle with long-term impacts of associated symptoms.
Especially over the course of a patient’s life, difficulties with executive functioning, emotional dysregulation, and sleep disturbance can manifest in many ways.
Studies have shown that anxiety exacerbates difficulties in inhibitory control and emotional regulation in children and adults.19
In addition, emotional regulation is dependent on sufficient cognitive resources, and heightened negative emotions can diminish executive function.20
In children with ADHD, sleep difficulties worsen ADHD symptom severity and neurocognitive deficits. In adults with ADHD, evidence suggests disturbed sleep is related to poorer collegiate academic functioning and a lower employment rate.21,22
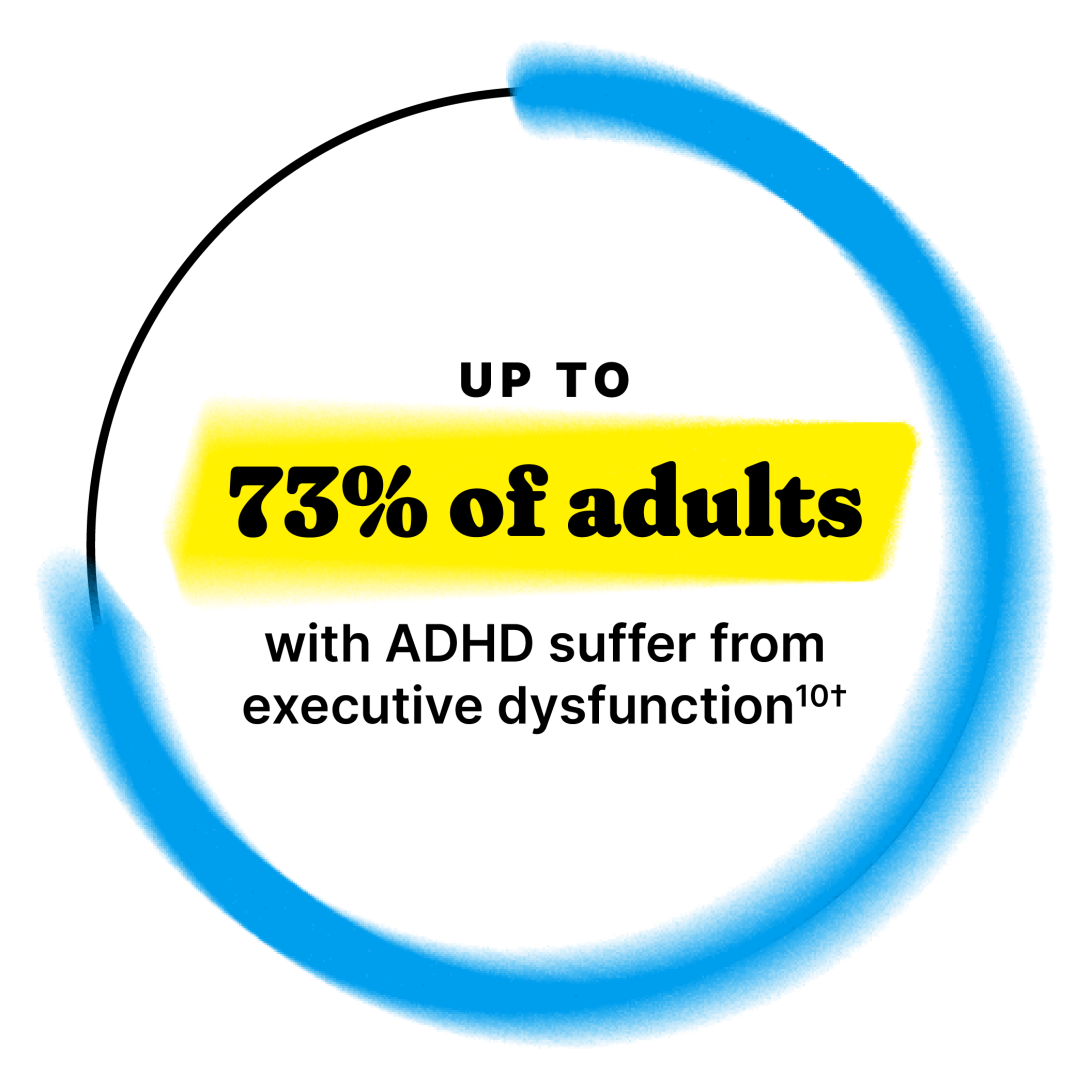
†Studies in adults with ADHD have reported executive function prevalence estimates of 30%-73%.
IT’S COMPLICATED
ADHD and comorbidities
Overlapping symptoms and shared pathophysiology between ADHD and other psychiatric disorders can complicate diagnosis and treatment.

get curious about ASSOCIATED SYMPTOMS
Explore resources to help better understand the impact of associated symptoms

Our understanding of ADHD is always evolving
Get the latest insights and resources delivered right to your inbox
-
1.
Brown TE, et al. Unmet treatment needs in adults with attention-deficit/hyperactivity disorder. Prim Care Companion CNS Discord. 2019;21(3):18m02397.
-
2.
Lenzi F, et al. Pharmacotherapy of emotional dysregulation in adults with ADHD: a systematic review and meta-analysis. Neurosci Biobehav Rev. 2018;84:359-367.
-
3.
Moukhtarian TR, et al. Effects of stimulants and atomoxetine on emotional lability in adults: a systematic review and meta-analysis. Eur Psychiatry. 2017;44:198-207.
-
4.
Centers for Disease Control and Prevention. Data and Statistics on ADHD. Published November 19, 2024. Accessed April 24, 2025.
-
5.
Jain R, et al. Addressing diagnosis and treatment gaps in adults with attention-deficit/hyperactivity disorder. Prim Care Companion CNS Disord. 2017;19:17nr02153.
-
6.
Shaw P, et al. Emotion dysregulation in attention deficit hyperactivity disorder. Am J Psychiatry. 2014;171(3):276-293.
-
7.
Katzman MA, et al. Adult ADHD and comorbid disorders: clinical implications of a dimensional approach. BMC Psychiatry. 2017;17(1):302.
-
8.
Holst Y, Thorell LB. Functional impairments among adults with ADHD: a comparison with adults with other psychiatric disorders and links to executive deficits. Appl Neuropsychol Adult. 2020;27(3):243-255.
-
9.
Arnold LE, et al. Long-term outcomes of ADHD: academic achievement and performance. J Atten Disord. 2020;24(1):73-85.
-
10.
Kosheleff AR, et al. Functional impairments associated with ADHD in adulthood and the impact of pharmacological treatment. J Atten Disord. 2023;27(7):669-697.
-
11.
Adler L, et al. The structure of adult ADHD. Int J Methods Psychiatr Res. 2017;26(1):e1555.
-
12.
Biederman J, et al. The effects of attention-deficit/hyperactivity disorder on employment and household income. Med Gen Med. 2006;8(3):12.
-
13.
Verheul I, et al. The association between attention-deficit/hyperactivity (ADHD) symptoms and self-employment. Eur J Epidemiol. 2016;31(8):793-801.
-
14.
Biederman J, et al. Impact of psychometrically defined deficits of executive functioning in adults with attention deficit hyperactivity disorder. Am J Psychiatry. 2006;163:1730-1738.
-
15.
Volkow ND, Swanson J. Clinical practice: adult attention deficit–hyperactivity disorder. N Engl J Med. 2013;369(20):1935-1944.
-
16.
American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. Fifth Edition, Text Revision. DSM-5-TR™. American Psychiatric Publishing; 2022.
-
17.
Brevik EJ, et al. Prevalence and clinical correlates of insomnia in adults with attention-deficit hyperactivity disorder. Acta Psychiatr Scand. 2017;136(2):220-227.
-
18.
Díaz-Román A, et al. Sleep in adults with ADHD: systematic review and meta-analysis of subjective and objective studies. Neurosci Biobehav Rev. 2018;89:61-71.
-
19.
Manoli A, et al. The differential effect of anxiety and ADHD symptoms on inhibitory control and sustained attention for threat stimuli: a go/no-go eye-movement study. J Atten Disord. 2021;25(13):1919-1930.
-
20.
Koay JM, Meter AV. The effect of emotion regulation on executive function. J Cogn Psychol (Hove). 2023;35(3):315-329.
-
21.
Lunsford-Avery JR, et al. Sleep disturbances in adolescents with ADHD: a systematic review and framework for future research. Clin Psychol Rev. 2016;50:159-174.
-
22.
Schein J, et al. Symptoms associated with ADHD/treatment-related adverse side effects and their impact on quality of life and work productivity in adults with ADHD. Curr Med Res Opin. 2023;39(1):149-159.
-
23.
Kessler RC, et al. The prevalence and correlates of adult ADHD in the United States: results from the national comorbidity survey replication. Am J Psychiatry. 2006;163(4):716-723.
-
24.
Danielson ML, et al. Prevalence of parent-reported ADHD diagnosis and associated treatment among U.S. children and adolescents, 2016. J Clin Child Adolesc Psychol. 2018;47(2):199-212.